Unraveling ALS: Causes, Symptoms, and Breakthroughs in Treatment
Amyotrophic lateral sclerosis (ALS), often referred to as Lou Gehrig’s disease, is a progressive neurodegenerative condition that affects nerve cells in the brain and spinal cord. This debilitating disease, named after the baseball player Lou Gehrig who was diagnosed in 1939, leads to the progressive degeneration and eventual death of motor neurons, which control voluntary muscles critical for movement, speech, and breathing.
What are the primary causes of ALS?
The exact cause of ALS remains elusive, but researchers have identified several factors that may contribute to its development. Genetic mutations play a role in about 5-10% of cases, particularly in familial ALS. Environmental factors such as exposure to certain toxins, heavy metals, and electromagnetic fields have been studied, but their direct link to ALS is not conclusively established. Additionally, factors like advanced age, military service, and smoking may increase the risk of developing ALS. Despite ongoing research, the majority of ALS cases are considered sporadic, with no clear cause identified.
How does ALS manifest as a silent invader of muscle weakness?
Muscle weakness is often the first noticeable symptom of ALS, earning it the moniker “Muscle Weakness A Silent Invader.” Initially, individuals may experience subtle changes in muscle strength, such as difficulty grasping objects or tripping more frequently. As the disease progresses, weakness spreads to other muscle groups, affecting limb movement, speech, and eventually breathing. This gradual onset can make early detection challenging, as symptoms may be attributed to other conditions or simply aging.
What are the early signs of ALS, including cramping?
Early signs of ALS can be subtle and vary from person to person. One common early symptom is muscle cramping, often referred to as “Cramped by Cramping Early Signs.” These cramps may occur in the arms, legs, or feet and can be particularly noticeable during physical activity or at rest. Other early indicators include muscle twitches (fasciculations), stiffness, and fatigue. As the disease progresses, individuals may notice difficulty with fine motor tasks, such as buttoning a shirt or turning a key. Recognizing these early signs is crucial for timely diagnosis and intervention.
How do speech and swallowing struggles impact ALS patients?
As ALS progresses, it often affects the muscles responsible for speech and swallowing, leading to “Speech and Swallowing Struggles.” Patients may experience slurred speech (dysarthria) or difficulty projecting their voice. Swallowing problems (dysphagia) can make eating and drinking challenging and increase the risk of choking or aspiration. These difficulties not only impact nutrition and hydration but also significantly affect communication and quality of life. Adaptive technologies and therapies can help manage these symptoms, allowing patients to maintain independence and social connections for longer periods.
Why is ALS considered the motor neuron enemy?
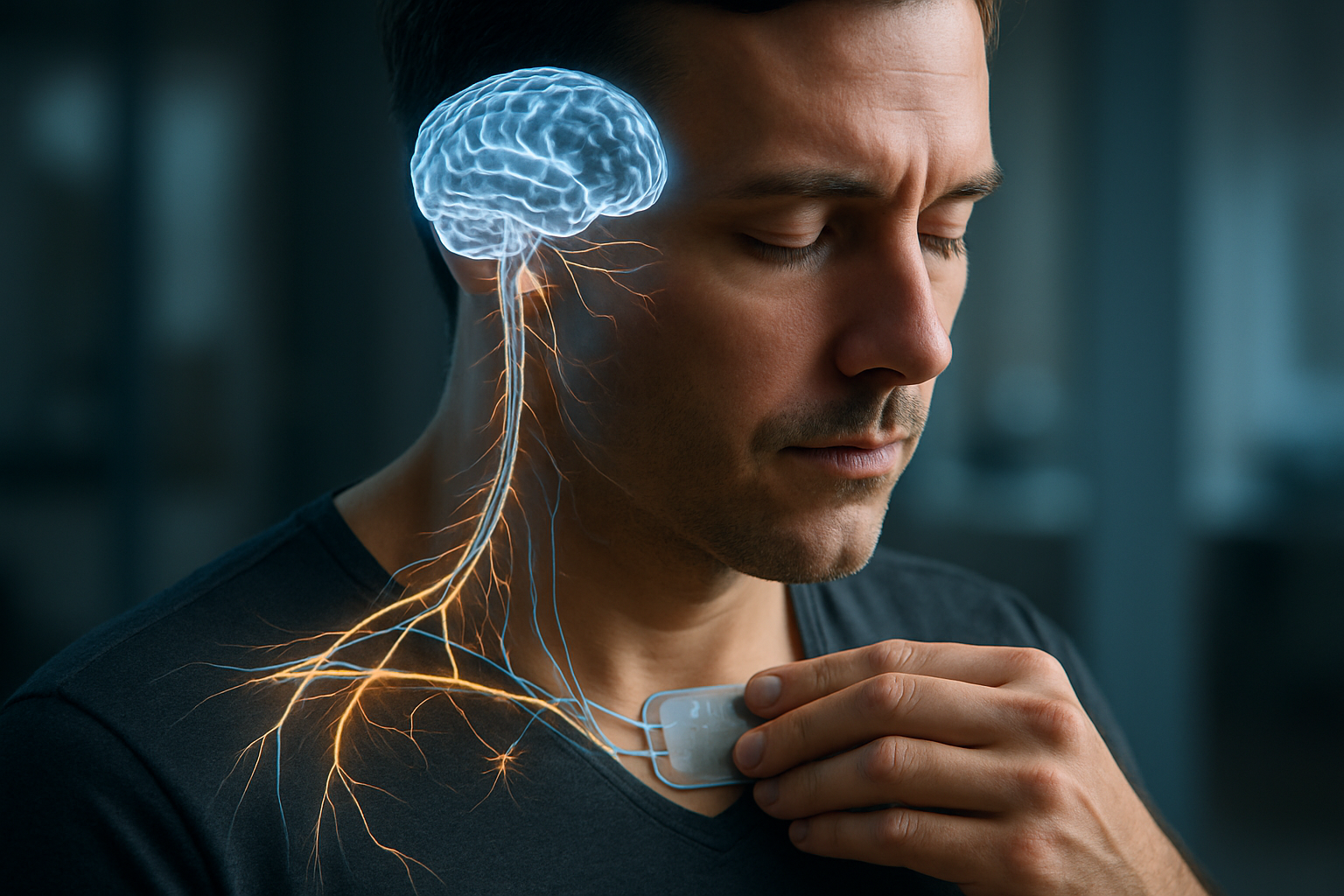
ALS is often described as “ALS The Motor Neuron Enemy” due to its selective attack on motor neurons in the brain and spinal cord. These neurons are responsible for transmitting signals from the brain to voluntary muscles throughout the body. As ALS progresses, it causes these neurons to degenerate and die, leading to a loss of muscle control and function. This relentless assault on motor neurons results in progressive paralysis, affecting movement, speech, and eventually breathing. The targeted nature of ALS on motor neurons makes it particularly devastating, as cognitive functions often remain intact while physical abilities decline.
What new hopes in research are emerging for ALS treatment?
The field of ALS research is dynamic, with “ALS Treatment New Hopes in Research” emerging regularly. Recent advancements include gene therapy approaches targeting specific genetic mutations associated with ALS. Stem cell therapies aim to replace damaged motor neurons or provide supportive cells to slow disease progression. Researchers are also exploring the potential of immunotherapy to modulate the immune system’s response in ALS. Additionally, new drug candidates targeting various aspects of ALS pathology, such as protein aggregation and neuroinflammation, are in clinical trials.
One promising area of research involves the use of antisense oligonucleotides (ASOs) to target genetic forms of ALS. This approach has shown success in treating spinal muscular atrophy, a related motor neuron disease, and is being adapted for ALS. Another innovative direction is the development of brain-computer interfaces that may help ALS patients communicate and control devices even as their physical abilities decline.
While there is currently no cure for ALS, FDA-approved treatments aim to slow disease progression and manage symptoms. Here’s a comparison of some current treatment options:
| Treatment | Type | Purpose | Estimated Monthly Cost |
|---|---|---|---|
| Riluzole | Oral medication | Slows disease progression | $600 - $1,000 |
| Edaravone (Radicava) | Intravenous infusion | Slows functional decline | $1,000 - $3,000 |
| Sodium phenylbutyrate-taurursodiol (Relyvrio) | Oral medication | Slows functional decline | $12,000 - $16,000 |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
As research continues to unravel the complexities of ALS, new treatment strategies and potential therapies offer hope for improved outcomes. While the road to a cure remains challenging, advancements in understanding the disease mechanisms and innovative approaches to treatment provide optimism for the ALS community. The combination of targeted therapies, supportive care, and emerging technologies aims to enhance the quality of life for those living with ALS and, ultimately, to find more effective ways to combat this devastating disease.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




