Macular Degeneration Unveiled: Key Insights on Prevention and Management
Macular degeneration is a common eye condition that leads to the deterioration of the macula, a small area in the retina responsible for central vision. This condition is a leading cause of vision loss, particularly among older adults. With the aging population, understanding macular degeneration, its risk factors, and how to manage and prevent it is essential.
What is age-related macular degeneration (AMD)?
Age-related macular degeneration (AMD) is a progressive eye disease that affects the central part of the retina, known as the macula. The macula is crucial for sharp, detailed vision needed for activities like reading, driving, and recognizing faces. As AMD progresses, it can lead to significant vision loss in the central field of view, while peripheral vision typically remains intact. AMD is the leading cause of severe vision impairment in adults over 60 in developed countries, making it a significant public health concern as populations age worldwide.
What are the main types of macular degeneration?
There are two primary types of macular degeneration: dry AMD and wet AMD. Dry AMD, also known as atrophic AMD, is the most common form, accounting for about 80-90% of cases. It develops slowly over time as the light-sensitive cells in the macula gradually break down. Wet AMD, also called neovascular AMD, is less common but more severe. It occurs when abnormal blood vessels grow under the retina and leak fluid or blood, causing rapid and severe vision loss. Understanding these types is crucial for proper diagnosis and treatment.
What are the risk factors for developing macular degeneration?
Unraveling risk factors for macular degeneration is essential for prevention and early intervention. Age is the most significant risk factor, with the likelihood of developing AMD increasing dramatically after age 50. Other risk factors include:
-
Genetics: Family history of AMD increases the risk.
-
Smoking: Doubles the risk of AMD and accelerates its progression.
-
Race: Caucasians are more likely to develop AMD than other races.
-
Obesity: Increases the risk and may accelerate AMD progression.
-
Cardiovascular diseases: Conditions like high blood pressure and high cholesterol are associated with increased AMD risk.
-
Diet: Low intake of antioxidants and omega-3 fatty acids may increase risk.
-
Sun exposure: Excessive UV light exposure may contribute to AMD development.
Understanding these risk factors can help individuals make informed lifestyle choices to reduce their risk of developing AMD.
What are the early signs of central vision decline?
Recognizing the early signs of central vision decline is crucial for timely intervention. Common symptoms of macular degeneration include:
-
Blurred or fuzzy vision, especially in the center of the visual field.
-
Difficulty reading or recognizing faces without extra light or magnification.
-
Straight lines appearing wavy or distorted (metamorphopsia).
-
Dark, blurry, or blank spots in the center of vision.
-
Colors appearing less vivid or faded.
-
Difficulty adapting to low light conditions.
-
Increased sensitivity to glare.
It’s important to note that these symptoms may develop gradually in dry AMD or appear suddenly in wet AMD. Regular eye exams are crucial for detecting AMD early, even before symptoms become noticeable.
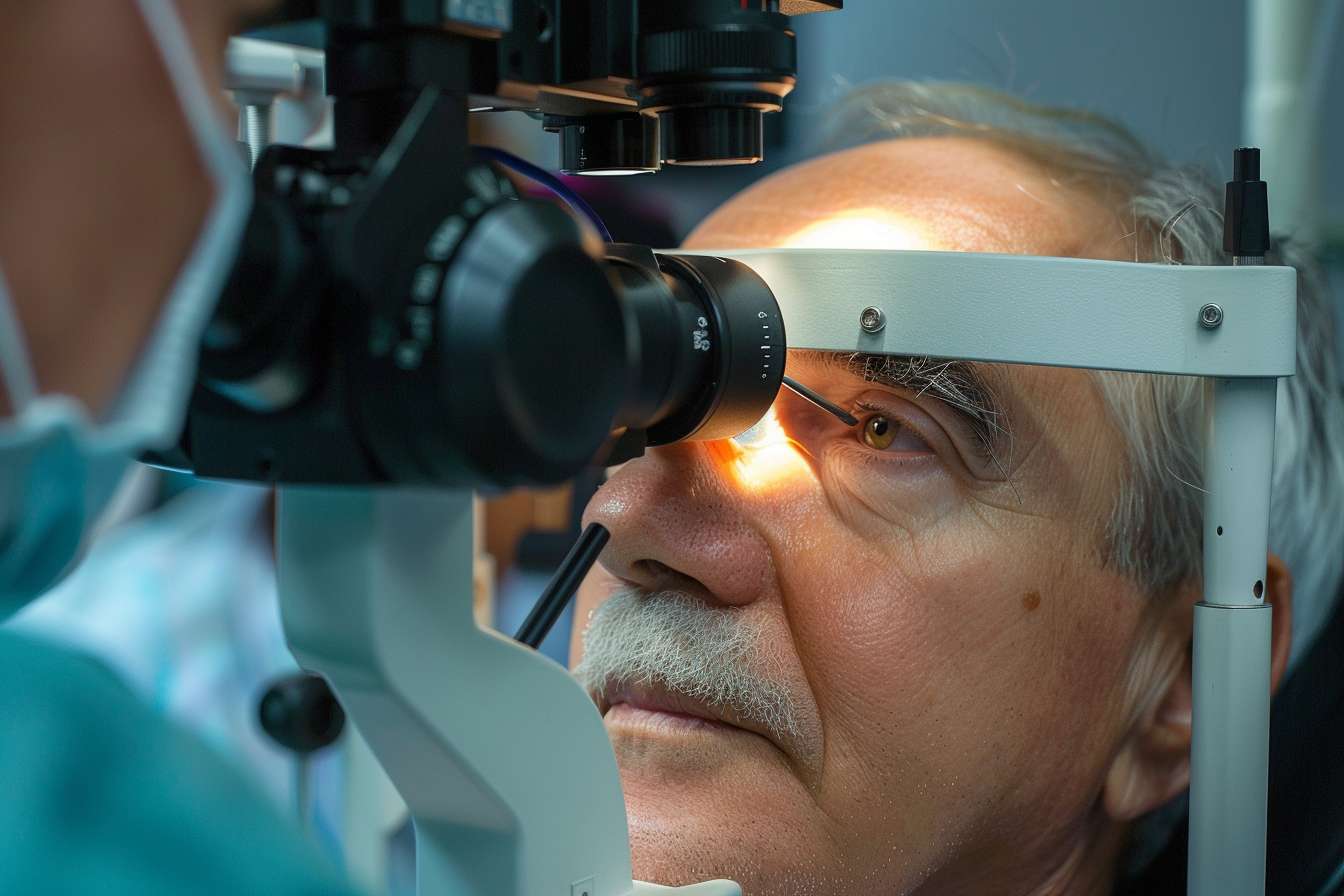
How is macular degeneration diagnosed and treated?
Diagnosis of macular degeneration typically involves a comprehensive eye exam, including visual acuity tests, dilated eye exams, and imaging tests such as optical coherence tomography (OCT) or fluorescein angiography. Once diagnosed, treatment options vary depending on the type and stage of AMD:
-
Dry AMD: Currently, there is no cure for dry AMD. Management focuses on slowing progression through lifestyle changes, such as quitting smoking, maintaining a healthy diet rich in antioxidants, and taking specific vitamin supplements (AREDS2 formula) as recommended by an eye care professional.
-
Wet AMD: Treatment options for wet AMD aim to stop abnormal blood vessel growth and include:
-
Anti-VEGF injections: Regular injections of medications that block vascular endothelial growth factor (VEGF) to prevent new blood vessel formation.
-
Photodynamic therapy: A combination of light-sensitive drugs and laser treatment to seal off leaking blood vessels.
-
Laser photocoagulation: Used in some cases to destroy abnormal blood vessels.
-
Early diagnosis and treatment are crucial for preserving vision and quality of life for individuals with AMD.
What strategies can help prevent and manage macular degeneration?
Preventing and managing macular degeneration involves a combination of lifestyle changes and regular medical care:
-
Regular eye exams: Schedule comprehensive eye exams, especially after age 50, to detect AMD early.
-
Quit smoking: If you smoke, seek help to quit as it significantly increases AMD risk.
-
Maintain a healthy diet: Consume a diet rich in leafy green vegetables, fish, and antioxidants.
-
Exercise regularly: Maintain a healthy weight and engage in regular physical activity.
-
Protect your eyes from UV light: Wear sunglasses and hats when outdoors.
-
Monitor your vision: Use an Amsler grid at home to detect changes in your central vision.
-
Control cardiovascular risk factors: Manage conditions like high blood pressure and high cholesterol.
-
Consider supplements: Discuss with your doctor whether AREDS2 supplements are appropriate for you.
-
Use low vision aids: If you have AMD, utilize magnifiers, special lighting, and other assistive devices to maintain independence.
-
Stay informed: Keep up with the latest research and treatment options for AMD.
By implementing these strategies, individuals can take proactive steps to protect their vision and manage macular degeneration effectively.
In conclusion, macular degeneration is a complex eye condition that can significantly impact quality of life. Understanding its types, risk factors, and early signs is crucial for prevention and timely intervention. With proper management strategies and regular medical care, individuals can work towards preserving their vision and maintaining their independence despite the challenges posed by AMD.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




